

- Medicare crossover definition manual#
- Medicare crossover definition verification#
- Medicare crossover definition plus#
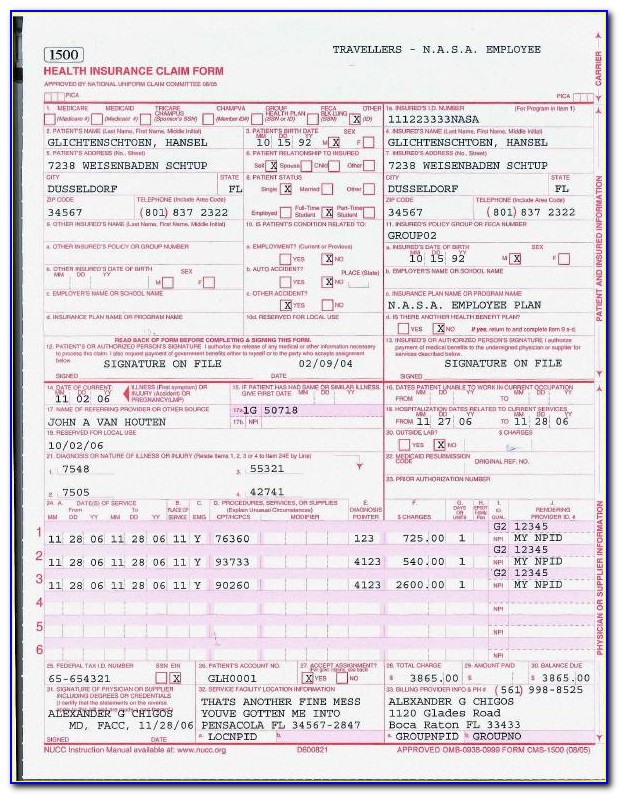
The following is an example of verifying eligibility when programs overlap: See Minnesota Health Care Programs (MHCP) chart on the Health Care Programs and Services webpage for more information on the programs. Overlapping MHCP and managed care organization (M CO) covera geĪ member could have both Medical Assistance and MinnesotaCare programs overlap for a short span in certain circumstances. MHCP will not inform providers of services the member is receiving from other providers. If the member is receiving the same services from another provider, the providers must coordinate the services and document in the member's record how the services were coordinated. Providers are responsible to ask MHCP members if they are currently receiving the same health care services from another provider. Please also review the following billing policies for all providers: Reconsideration of a Claim (Appeals vs.Overlapping MHCP and managed care organization (MCO) coverage.This section outlines the following for all MHCP providers: Minnesota’s Uniform Electronic Transactions and Implementation Guide Standards (PDF) require all Minnesota-based health care claims to be submitted electronically.
Medicare crossover definition verification#
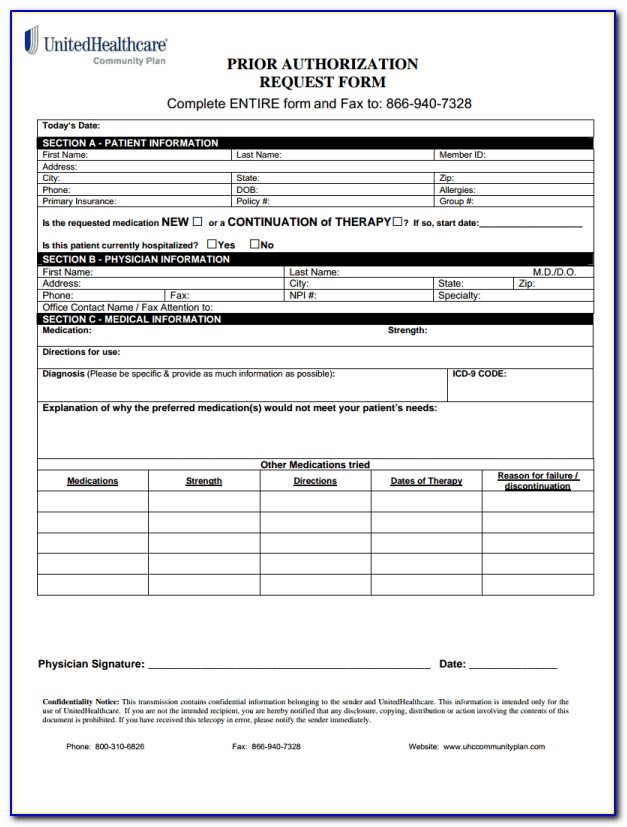
The federal Health Insurance Portability and Accountability Act of 1996 (HIPAA) requires all health care providers and payers to use universal standards for electronic billing and administrative transactions (health care claims, remittance advice, eligibility verification requests, referral authorizations and coordination of benefits). Contact the appropriate MCO to learn about the billing policies for services provided to MCO-enrolled MHCP members. MHCP members enrolled in a managed care organization (MCO) contracted with MHCP receive their health care services through the MCO.
Medicare crossover definition manual#
Minnesota Health Care Programs (MHCP) providers and their billing organizations must follow MHCP billing policies as outlined in this section and provider type specific sections of the MHCP Provider Manual for billing services provided to FFS members. Call 1-85, TTY 711 from 8 am – 8 pm local time, seven days a week for more information.In a fee-for-service (FFS) delivery system, providers (including billing organizations) bill for each service they provide and receive reimbursement for each covered service based on a predetermined rate. This information is not a complete description of benefits. Enrollment in the plan depends on the plan’s contract renewal with Medicare and a contract with the State Medicaid Program. Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. You can find complete information about dual plans available your area at Or call 1-85, TTY 711 from 8 am – 8 pm local time, seven days a week. People who qualify for a dual plan can enroll or switch to a new plan at certain times throughout the year, not just during the Annual Enrollment Period.
Want to get extra benefits and features? See if you qualify. That makes a dual plan a low-cost choice too.

Medicare crossover definition plus#


 0 kommentar(er)
0 kommentar(er)
